Intracardiac Robotic Surgery Program Development
-
We build a customized plan based on the team skills and needs:
Peer-to-Peer Training: Involves Surgeon, Anesthesia, Perfusion, Scrub, First Assistant, and Circulating RN to cover all aspects of the surgical algorithm.
CT Scan Review: Conduct comprehensive assessments to ensure crucial imaging is appropriately integrated into surgical planning.
Perfusion Plan Development: Options for femoral or axillary access to tailor the perfusion strategy.
Chest Port Access Assessment: Determining the most suitable approach between ports and thoracotomy.
Clamp and/or Endo-balloon Training: Assistance with clamp techniques and training on the Endo-Balloon to enhance procedural competency and expand applicability to a greater pool of patients.
Decision-Making Skills Enhancement: Focus on the use of clamps or Endo Balloon, stressing the importance of informed decision-making.
Myocardial Protection Techniques: Training to implement effective myocardial protection strategies.
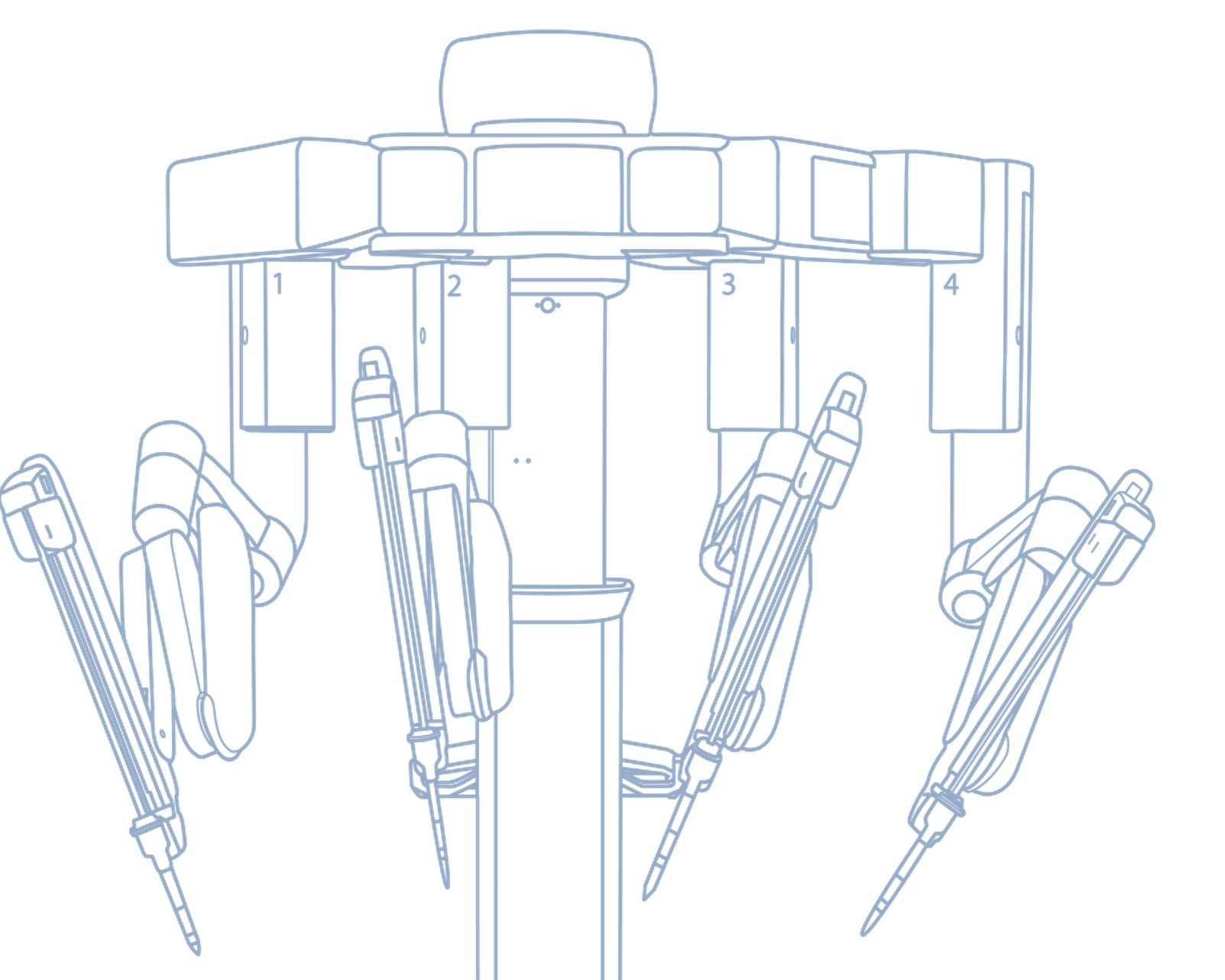
Robotic Instrument Usage: Detailed guidance on robotic instrument needs and their application.
Conventional and Robotic Tasks: Integration of conventional mitral tasks with re-engineered robotic procedures.
Robotic Setup: Preparation for a robotic operating room environment, ensuring readiness for robotic-assisted surgeries.
Cardiac Anesthesia Training: Covering double lumen tube techniques and TEE (Transesophageal Echocardiography) use.
Skills Drills for Entire Team: Regular practice sessions for all team members to enhance competency.
Proctoring Support: Available for Surgeons and First Assistants during live cases at your hospital.
Ongoing Support: Extended assistance for a duration of 3-6 months to ensure seamless integration of new procedures.
Optional Dashboard Development: A tool to track and evaluate the progress of your program.
-
The ports-only approach in robotic surgery shows significant advantages for various patient populations, enhancing its applicability across a wide range of clinical scenarios. This technique is particularly beneficial for up to 97% of patients seeking robotic interventions, providing effective solutions for those with complex medical histories, including:
Redo Surgeries: For patients requiring reoperation, the ports-only approach minimizes complications associated with traditional incision methods, facilitating safer and more efficient restaging of procedures.
Previous Sternotomy: Patients who have undergone prior sternotomies often present unique challenges due to scar tissue. The ports-only technique helps to navigate these areas more effectively, reducing the risk of damage to surrounding structures.
Morbidly Obese Individuals: The minimally invasive nature of the ports-only approach is particularly advantageous for morbidly obese patients, where traditional methods can pose higher risks. This approach leads to reduced postoperative pain, quicker recovery times, and shorter hospital stays.
Patients with Previous Stroke: For individuals with a history of stroke, the ports-only technique reduces stress and strain on the body compared to more invasive methods, aligning with the surgical needs of these patients while prioritizing safer outcomes.
Overall, the ports-only approach expands the accessibility of robotic surgeries, making advanced treatment options available to a broader range of patients, while maintaining safety and efficacy.
-
The organization of a robotic operating room (OR) as a microsystem has been shown to enhance surgical efficacy while minimizing morbidity and mortality rates. This model allows for structured interactions among various components, leading to optimized workflows and improved patient outcomes. By applying a similar microsystem approach to robotic minimally invasive (MV) programs, either through the full integration of all necessary elements or through the selective implementation of key components, organizations may achieve enhanced safety and long-term sustainability. Such strategies could facilitate the adoption of robotic techniques across different surgical disciplines, ultimately contributing to more effective healthcare delivery and better resource management in surgical settings. -
Item Roadmap for Maximizing the Digital Robotic Operating Room
1. Assessment of Surgical Methods
Identify Variabilities: Collaborate with surgeons to document specific surgical methods and variations.
Standardization of Processes: Create a baseline of practices to ensure a consistent starting point for all surgical teams.
2. Customized Role-Based Checklists
Develop Checklists: Create detailed checklists for each surgical role (e.g., lead surgeon, anesthesiologist, scrub nurse) tailored to the identified surgical methods.
Incorporate Best Practices: Include insights from past procedures to minimize intraoperative communication and potential errors.
3. Training and Education
Team Training Sessions: Implement regular training schedules for all operating room personnel on the use of TileProTM and robotic systems.
Simulation Exercises: Use simulation technology to allow team members to practice procedures in a risk-free environment.
4. TileProTM Setup
Initial Configuration: Ensure TileProTM is set up according to the specific needs of each surgical method, focusing on both safety and efficacy.
User Interface Training: Train surgical teams on utilizing the TileProTM interface to facilitate seamless interactions during surgery.
5. Communication Protocols
Streamlined Communication Systems: Develop protocols for intraoperative communication to ensure clarity and efficiency among team members.
Feedback Mechanism: Establish a method for collecting real-time feedback during operations to improve checklist effectiveness and team coordination.
6. Continuous Improvement
Post-Procedure Analysis: Conduct debrief sessions to evaluate the effectiveness of checklists and TileProTM setups after operations.
Iterative Updates: Regularly update the checklists and procedures based on team feedback and changes in surgical practices.
7. Documentation and Reporting
Documentation Standards: Implement standards for documenting procedures and checklist adherence to provide accountability.
Performance Metrics: Establish metrics to evaluate the success of the setup process and surgical outcomes.
8. Review and Adaptation
Regular Reviews: Schedule periodic reviews of checklists and operating procedures to adapt to new technologies and surgical techniques.
Stakeholder Involvement: Engage all stakeholders, including surgeons, nurses, and administrative staff, in revisions to ensure comprehensive input.
This strategic roadmap aims to leverage the capabilities of the digital robotic operating room and enhance communication and safety through tailored checklists and effective team education.
-
The concept of using a checklist in the robotic operating room (OR) was inspired by Dr. Murphy’s experience in aviation, where checklists are critical for ensuring safety and precision. This philosophy is deeply rooted in our commitment to achieving zero acceptable losses in patient care. By adopting a systems approach that incorporates a role-based checklist, we enhance patient safety and systematically reduce the likelihood of errors.
In the high-stakes environment of the OR, where complexities abound and stakes are high, a checklist serves as an essential tool. It ensures that all team members—surgeons, nurses, scrub, perfusion, anesthesia —are aligned and accountable for their responsibilities. Each item on the checklist is designed to cover critical steps in the surgical process, promoting thoroughness and attention to detail.
Evidence has shown that the use of checklists in medical settings can significantly decrease complications and improve outcomes. By rigorously adhering to a systematic protocol, teams can identify and address potential issues before they escalate into problems, ultimately leading to better patient safety and care quality.
Implementing this approach not only nurtures a culture of safety within the robotic OR but also emphasizes teamwork and communication. It reiterates the importance of every role and fosters an environment where all personnel feel empowered to contribute to patient outcomes actively. As we continue to innovate in the field of robotics and surgical practices, our role-based checklists will remain a cornerstone of our commitment to excellence in patient care.
Our team will devise a customized check list based on the surgeon’s individual technique and surgical steps. This checklist will then be visible on individual screens throughout the OR and advance in tandem.
-
We can customize an approach that meets your unique needs and expertise. By incorporating our solutions, you can anticipate recovering your investment quickly, typically with only 2-4 cases that may not have reached your facility otherwise.